How does
photodynamic therapy work?
Photodynamic therapy (PDT) uses natural dyes and light to gently destroy cancer cells. The dyes are called “photosensitizers” or “photosensitizers” (PS) because they are taken up into cancer cells and make them sensitive to light of certain wavelengths.
Photodynamic therapy has a long history of nearly 100 years and has been used successfully for some time to treat a variety of tumors. In particular, superficial tumors in the skin, lungs, intestines and urinary bladder are easily accessible to the irradiated light. However, tumors in solid organs such as the kidney or bladder can also be treated with PDT.
How does
PHOTODYNAMIC THERAPY
affect CANCER?
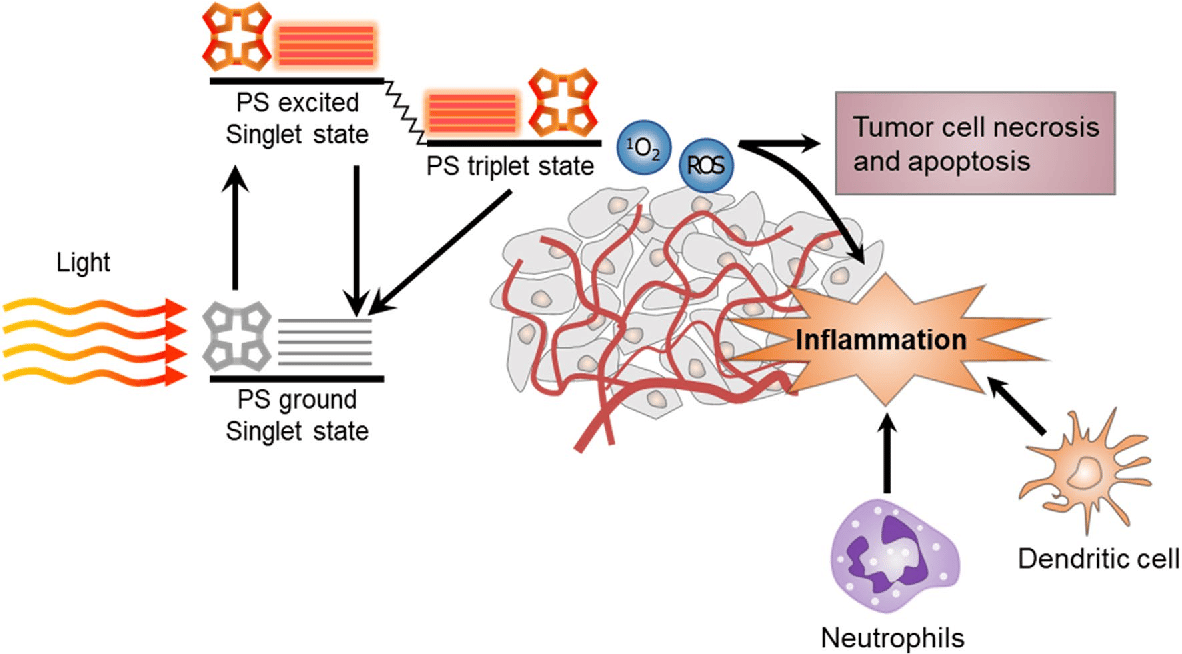
When a cancer cell that has taken up the photosensitizer is irradiated with light of a certain wavelength, the light energy triggers chemical processes that lead to the formation of oxygen compounds, especially oxygen radicals, which are highly toxic to cells and kill the cell.
In general, photosensitizers are initially taken up by all cells. But the accumulation of PS in tumor cells is higher than in normal body cells, so that, depending on the type of PS, 10-20 times higher concentrations can be reached in cancer cells. Accordingly, when irradiated with light, tumor cells primarily die off, while normal cells survive.
Depending on the PS and type of treatment, PDT may also damage blood vessels in the tumor, cutting off the blood supply to the tumor, without which the tumor cannot grow.
In addition, PDT triggers an immune response against the tumor cells by causing the dying tumor cells to release tumor antigens that are recognized by the immune system – similar to a vaccination. These tumor antigens enable the killer cells of the immune system to find and destroy the tumor cells in the body.
How is
photodynamic therapy
carried out?
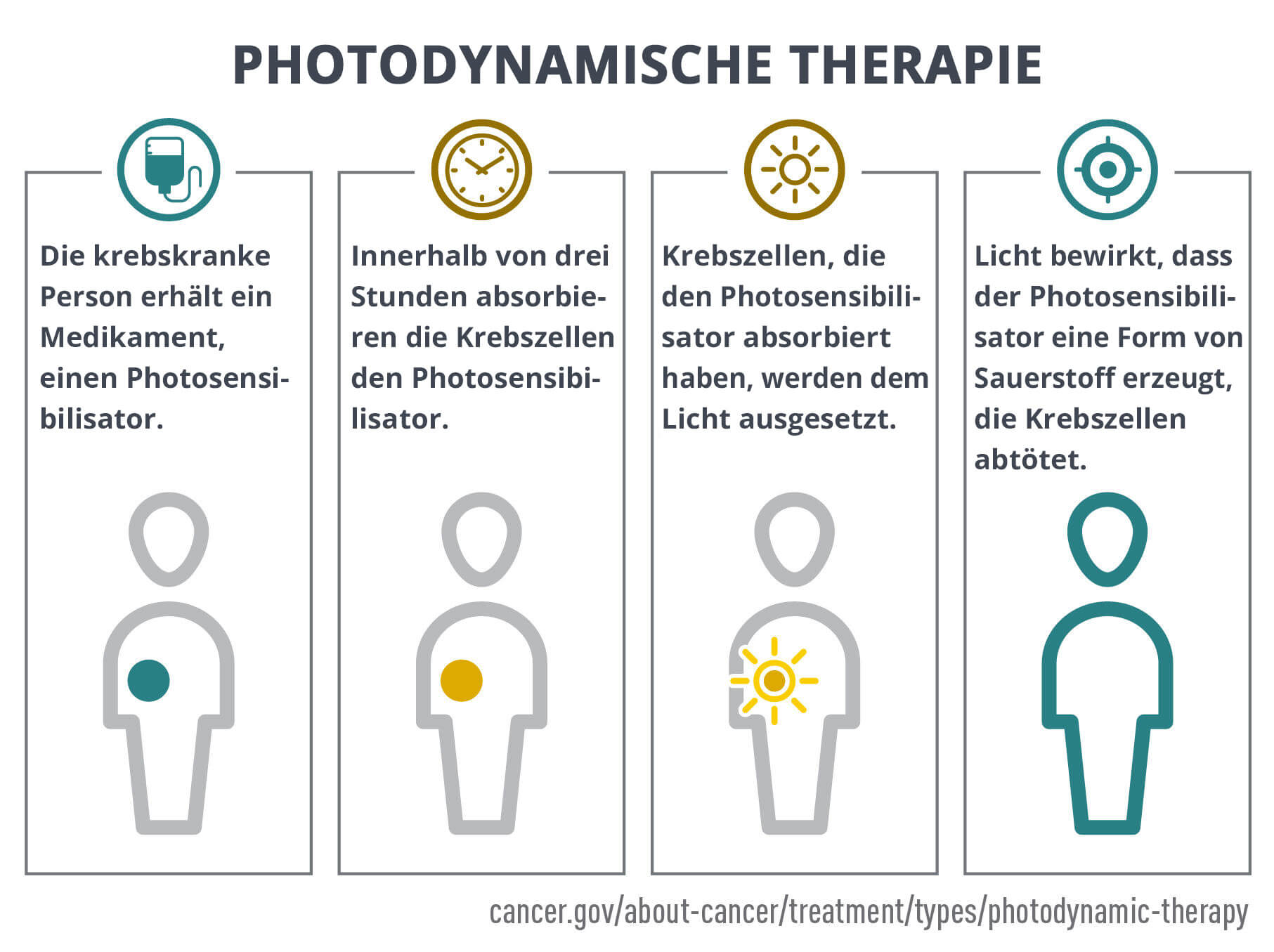
PDT is a two-step process. First, the photosensitizer is applied. This is usually done by intravenous infusion, but can also be done by local injection into the tumor or instillation into a holhl hollow space such as the bladder.
Hours or days later, depending on the accumulation behavior of the photosensitizer, the PS has accumulated in cancer cells. By this time, however, the PS has already left normal cells – through metabolic and/or transport processes.
In the second step, the cells are exposed to the light of a specific wavelength absorbed by the PS, which activates the PS and destroys the cell. Due to the selective accumulation in the cancer cells, primarily the tumor is destroyed, while normal tissues and cells are spared.
Call us now on +49 (0)177 23 82 863 or get in touch using the contact form
Advantages of
photodynamic
therapy
PDT primarily destroys tumor cells and spares normal cells and tissue.
In addition, PDT destroys cells without heating, unlike widely used thermal ablation techniques such as radiofrequency ablation (RF ablation) and High-Energy Focussed Ultrasound (HiFU). Thus, PDT preserves the tissue infrastructure of fibers and interstitial matrix, as well as nerves and vessels. This enables functional preservation of anatomical structures: in the case of bladder treatment, among other things, preservation of penile erectile function by preserving the neurovascular bundle, a vascular and nerve plexus on the bladder that is destroyed during HiFU treatment or surgical removal of the bladder. The bladder sphincter can also be preserved during PDT treatment, even with partial infiltration by tumor tissue if necessary.
Also, PDT minimizes scarring and induces strong secondary immune effects against cancer cells.
Disadvantages of
photodynamic
therapy
PDT, despite selective accumulation in tumor cells, can also damage normal cells and tissues and cause side effects.
In most cases, the light can only penetrate solid tissue to a depth of about 1 cm during PDT and can only destroy cells to this depth. When treating solid tumors of larger dimensions, many light sources – usually fiber optic light guides – must be inserted into the tumor at intervals of 1 cm to illuminate the entire tumor mass.
Potential
side effects of
photodynamic
therapy
Damage to normal cells from PDT, although limited, can result in burn-like symptoms, swelling, pain, and scarring m the treatment area. Other potential side effects, depending on the area of the body being treated, include:
- Cough
- Difficulty swallowing
- Stomach pain
- Pain when breathing
- Shortness of breath
- Skin problems such as redness, stinging, swelling or itching
Photodynamic Therapy with CHlorin E6 for Bladder Vancer
In the treatment of bladder cancer with photodynamic therapy (PDT), the photosensitizer chlorin E6 is initially administered as a short infusion. This substance is distributed throughout the body via the bloodstream, but accumulates around 20 times more in tumor tissue than in healthy cells.
After a certain waiting period, during which chlorin E6 has selectively accumulated in the tumor tissue of the bladder, irradiation with red laser light takes place. The laser light is introduced into the bladder via thin light guides (glass fibers). This can be done via a catheter or a flexible cystoscope, which is used to reach the bladder in a minimally invasive way.
The laser light activates the photosensitizer in the tumour cells, producing toxic oxygen radicals that specifically destroy the cancer cells. Healthy tissue is largely spared as it has absorbed less or no photosensitizer.
This method is particularly suitable for flat or locally advanced tumors in the bladder mucosa and can even be used for muscle-invasive tumors in certain cases – provided that the light guides can be brought sufficiently close to the tumor tissue.
What is Chlorin E6 and how does it work?
Chlorin E6 is a natural photosensitizer obtained from plant material. It is a green porphyrin that accumulates strongly in tumor tissue. If the enriched tumor tissue is irradiated with monochromatic laser light of 665 nanometers (red light), the light energy is transferred to the chlorin E6 molecule.
The absorbed energy is then transferred to oxygen molecules in the cell, creating highly reactive oxygen radicals. These destroy vital structures of the tumor cell, such as the cell nucleus, cell membrane and mitochondria, thereby specifically killing the cancer cell.
Healthy cells that contain little or no chlorin E6 are not damaged by the light – this is what makes this therapy so selective.
Call us now on +49 (0)177 23 82 863 or get in touch using the contact form
Other photodynamic
therapy methods for
bladder cancer
In addition to chlorin E6, other photosensitizers have also been tested for PDT in bladder cancer, for example 5-aminolevulinic acid (5-ALA). This substance can be instilled (flushed) into the bladder and is absorbed directly by the bladder cells. It is particularly suitable for flat, superficial tumors of the bladder mucosa (e.g. carcinoma in situ).
In contrast, Chlorin E6 is also suitable for infiltrative tumors that have grown deeper into the bladder wall due to its stronger depth effect.
Other PDT methods such as Tookad, which is mainly used for prostate cancer, do not play a role in the treatment of bladder cancer as they are based on a different mechanism of action and do not accumulate sufficiently selectively in the bladder tissue.
For which bladder cancer patients
is photodynamic therapy particularly suitable?
In contrast to surgical, chemotherapeutic or radiotherapeutic procedures, PDT represents a significantly lower burden for the patient.
Although no clinical studies are available to date to indicate in which cases of bladder cancer photodynamic therapy is particularly suitable, it can be deduced on the basis of the fewer side effects of PDT that it is particularly suitable for the treatment of bladder tumors if the affected man wishes to avoid side effects such as impotence and incontinence.
PDT should also be considered and weighed against alternatives such as IRE or electrochemotherapy (ECT) for tumors infiltrating critical strictures such as the bladder sphincter or bladder floor.
PDT also represents a therapeutic problem-solving alternative for patients who are considered “out of treatment” in the “conventional medical sense” or for patients who reject conventional therapies.
Other cancers and precancerous lesions treated with photodynamic therapy
The U.S. Food and Drug Administration (FDA) has cleared photodynamic therapy for the treatment of the following conditions:
- Actinic keratosis
- Advanced cutaneous T-cell lymphoma
- Barrett esophagus
- Basal cell carcinoma of the skin
- Esophageal Cancer
- Non-small cell lung cancer
- Squamous cell carcinoma of the skin (stage 0)
PDT is also used to relieve the side effects of the following cancers (palliative, not curative).
- Esophageal cancer when it blocks the esophagus
- Non-small cell lung cancer when it blocks the airways
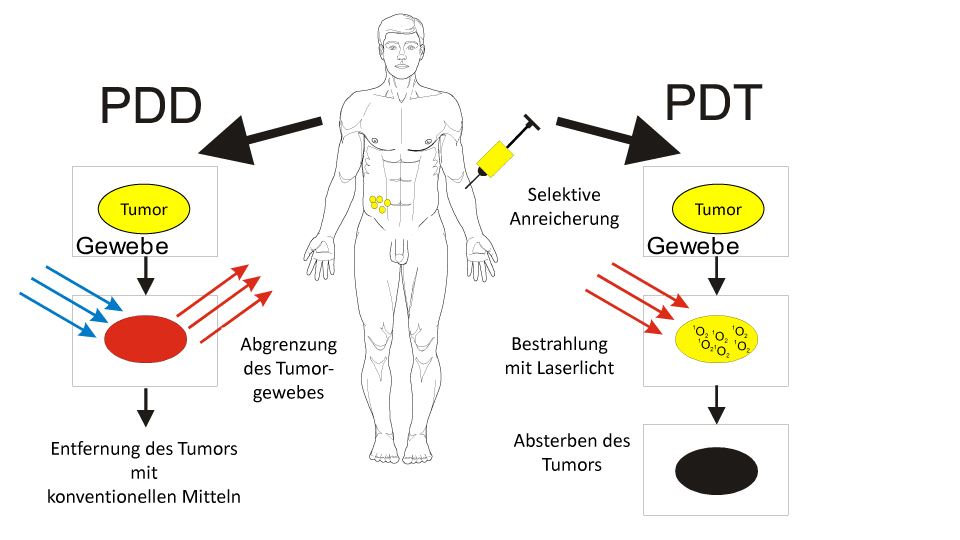
Photodynamic therapy (PDT) is then also possible with Chlorin E6 (right part of the illustration). Three hours after the injection of Ce6, the tumor cells took up the substance. Irradiation with special laser light triggers a chemical reaction in the tumors, producing singlet oxygen.


